
Staphylococcal pneumonia
Staphylococcus aureus pneumonia is a serious but relatively uncommon disease with a high case fatality rate. It often complicates influenza. The special relationship of staphylococci and influenza virus has been dealt with on page 158. In children, staphylococcal pneumonia may follow measles or whooping cough. In infants a primary staphylococcal bronchopneumonia is known, with a case fatality rate as high as 80% in the pre-antibiotic era. The infection is generally endogenous, the bacteria frequently being derived from the patient’s skin or nose and the infection air-borne. However, staphylococcal pneumonia or lung abscess sometimes follows bacteraemia or septicaemia,37 particularly in drug addicts with right-sided bacterial endocarditis.
S. aureus can also cause serious infections such as pneumonia (infection of the lungs) or bacteremia (bloodstream infection). Symptoms of these infections include: difficulty breathing, malaise, fever, or chills.
Staphylococcal pneumonia is a disease process that requires prompt diagnosis, as sequelae can lead to complications such as severe necrotizing pneumonia, bacteremia, or sepsis with or without shock. Staphylococcal pneumonia can be seen in a post-viral state. This activity reviews the evaluation and treatment of staphylococcal pneumonia and highlights the role of the interprofessional team in evaluating and treating patients with this condition.
Treatment / Management
Treatment for staphylococcal pneumonia depends on if this process is categorized into either MRSA or MSSA. If MRSA is suspected or confirmed, either vancomycin or linezolid should be initiated at the start of treatment and be promptly discontinued if MRSA is ruled out. Both vancomycin and linezolid have similar efficacy, and selection should be based on patient tolerance, antibiotic allergy profile, renal function, drug interaction, and intravenous access. As linezolid is systemically bioavailable in its oral form, this is preferred if there is an issue with intravenous access. Vancomycin is preferred if the patient is cytopenic or taking selective serotonin reuptake inhibitors (SSRIs).[12][13] Ceftaroline can be used if vancomycin or linezolid are contraindicated; however, it should be known that it is not FDA approved for hospital-acquired pneumonia or ventilator-associated pneumonia. Clindamycin is also an alternative, but it is also less efficacious in hospital-acquired and ventilator-associated pneumonia.[14]
If culture results grow MSSA and rule out other causes of pneumonia, then therapy can be de-escalated to nafcillin, oxacillin, or cefazolin.[15] Supportive measures for staphylococcal pneumonia include bronchodilation to help those with underlying lung diseases such as asthma or chronic obstructive pulmonary disease (COPD). Supplemental oxygenation may also be needed due to the restrictive lung disease caused by the pneumonia disease process. This can begin with a nasal cannula. However, if the disease process is severe enough, then mechanical ventilation may be necessary.

Differential Diagnosis
As the clinical presentation for pneumonia and, therefore, staphylococcal pneumonia is broad and nonspecific, so is the differential for this process. Differential diagnosis may include:
- Pneumonia secondary to:
- Streptococcal pneumonia
- Nontypeable Haemophilus influenza
- Mycoplasma pneumonia
- Chlamydia pneumonia
- Legionella
- Gram-negative bacilli
- Group A Streptococcus
- Anaerobic infection
- Mycoplasma tuberculosis
- Viral infection
- Pulmonary edema secondary to congestive heart failure
- Pulmonary hemorrhage
- Atelectasis
- Pneumonitis from aspiration or chemical exposure
- Interstitial lung disease
- Drug reaction
- Pulmonary embolism
Overview - Staphylococcal pneumonia
Infectious diseases
Bryan Corrin MD FRCPath, Andrew G. Nicholson DM FRCPath, in Pathology of the Lungs (Third Edition), 2011
Staphylococcus aureus pneumonia is a serious but relatively uncommon disease with a high case fatality rate. It often complicates influenza. The special relationship of staphylococci and influenza virus has been dealt with on page 158. In children, staphylococcal pneumonia may follow measles or whooping cough. In infants a primary staphylococcal bronchopneumonia is known, with a case fatality rate as high as 80% in the pre-antibiotic era. The infection is generally endogenous, the bacteria frequently being derived from the patient's skin or nose and the infection air-borne. However, staphylococcal pneumonia or lung abscess sometimes follows bacteraemia or septicaemia,37 particularly in drug addicts with right-sided bacterial endocarditis.
Although the mortality from most forms of pneumonia has been reduced by modern drugs, many strains of Staphylococcus now widely distributed in the population are resistant to the generally used antibiotics. Even relatively new antibiotics such as meticillin are inactive against some of these staphylococci, which have become known as meticillin-resistant S. aureus or MRSA. Such strains periodically become prevalent in hospitals,15 carried in the nose by staff and patient, and fatalities from staphylococcal infection, often with pneumonia, have occurred among surgical patients who otherwise should have recovered from their operation. In addition, although MRSA is primarily viewed as the prototype of multiresistant nosocomial (hospital-acquired) infections, new lineages have emerged that cause community-acquired infections in individuals without risk factors, including rare cases of necrotising pneumonia.38–40
S. aureus owes its pathogenicity to a series of necrotising exotoxins that induce a marked neutrophil response resulting in suppurative tissue necrosis.41 Particularly potent is a strain of meticillin-resistant S. aureus that secretes an exotoxin known as Panton–Valentine leukocidin. As well as complicating influenza,42–44 this strain has resulted in fatal septic shock in previously healthy persons.38
At necropsy, the bronchi are acutely inflamed and the lungs contain many bright yellow centrilobular foci of suppuration (Fig. 5.2.7), which in the more advanced cases may have enlarged and coalesced to form abscesses 1 cm or more in diameter. Adjacent air spaces contain a purulent exudate. A superficial abscess may rupture into the pleura and cause empyema, which is a common complication of staphylococcal pneumonia. If the patient survives, there may be permanent damage to the lungs in the form of pulmonary fibrosis, bronchiectasis or large air-filled cysts known as pneumatoceles (Fig. 5.2.8).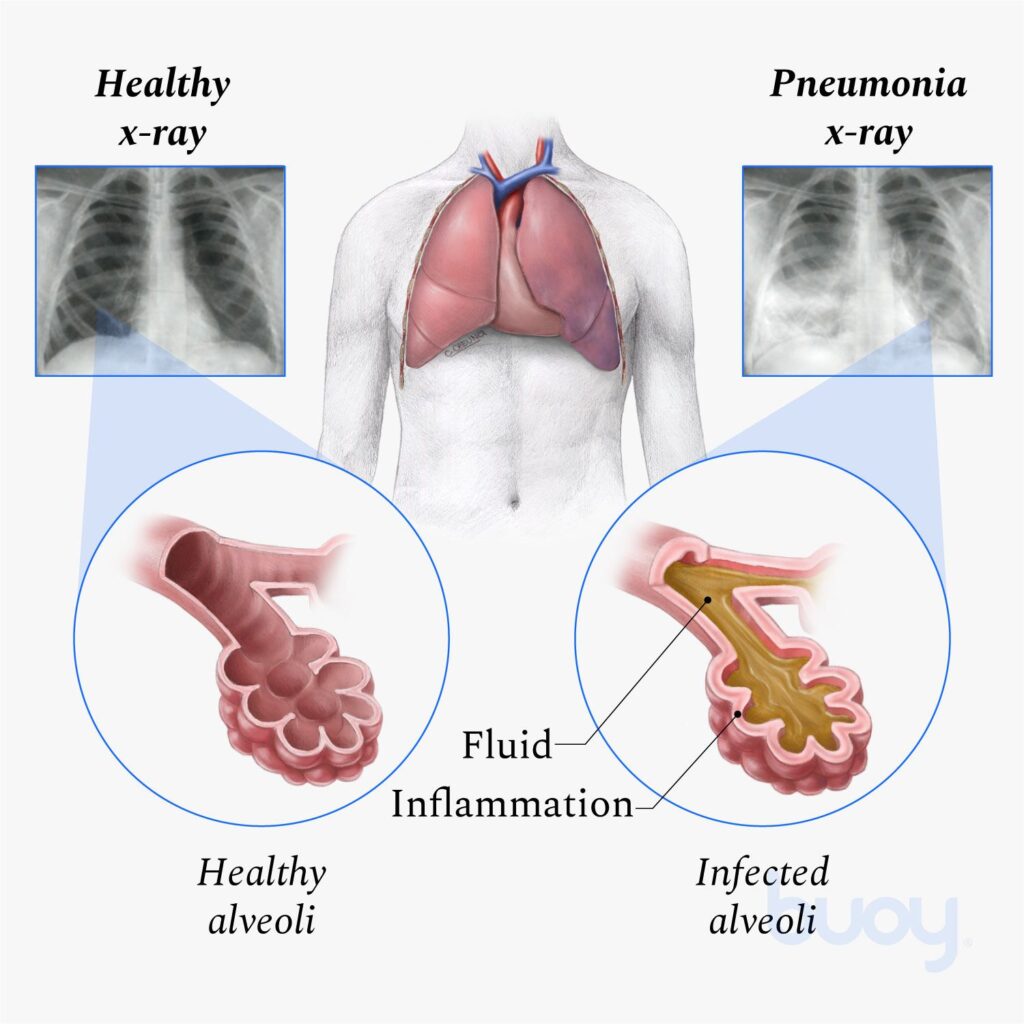
Bacterial Diseases
Carol F. Farver, in Pulmonary Pathology (Second Edition), 2018
Microscopic Findings
Staphylococcal pneumonia can be acquired hematogenously or as a bronchopneumonia (Fig. 10.6) that may arise out of an acute, necrotizing tracheobronchitis, which spreads distally to involve the alveoli. This acute, exudative infiltrate usually expands to fill large areas of the surrounding lung and commonly develops into a necrotizing pneumonia with cavitation and abscess formation (Fig. 10.7). Within the phagocytes of the infiltrates, gram-positive cocci are abundant, usually in grapelike clusters. Though pleuritis is uncommon, extension of these cavities to the pleural surface and empyema formation are common.
Pneumonitis and Interstitial Disease
Jeffrey C. Benson, … Tom B. Rice, in Pediatric Critical Care (Fourth Edition), 2011
Staphylococcal Pneumonia
Primary S. aureus pneumonia has decreased in frequency in recent years but still accounts for approximately 25% of cases in young infants. The incidence of secondary or metastatic dissemination has increased since 1972. Patients with primary pneumonia present with fever and respiratory symptoms, whereas those with metastatic disease often present with fever, generalized toxicity, and musculoskeletal symptoms. In patients presenting with primary staphylococcal pneumonia, the disease often is preceded by an upper respiratory tract infection.40,41 Pleural effusion or empyema develops in nearly 80% of the patients with primary staphylococcal pneumonia and is extremely common in patients with metastatic disease. It is not unusual for patients with staphylococcal pneumonia to remain bacteremic long after the initiation of appropriate antibiotic therapy.
Radiographic findings of S. aureus pneumonia differ according to the stage of disease. They vary from minimal changes to consolidation (most common) and are associated with pleural effusion (50% to 60%) or pneumothorax (21%). Pneumatoceles usually appear during the convalescent stage and may persist for prolonged periods in asymptomatic patients. Antibiotic therapy should be administered intravenously and include a drug that is resistant to inactivation. Strong consideration should be given to providing antibiotic coverage for methicillin-resistant S. aureus, which can account for 1% to 30% of isolates, depending on the prevalence in the area.42 The duration of therapy usually is lengthier in patients with staphylococcal disease than for patients with other bacterial pneumonias and consists of 21 days or more of treatment. The mortality rate of staphylococcal pneumonia varies from 23% to 33%. An increased incidence of mortality usually is associated with younger age, inappropriate initial antimicrobial therapy, or failure to drain an empyema appropriately.
Bacterial Pneumonia
W Abdullah Brooks, in Hunter’s Tropical Medicine and Emerging Infectious Disease (Ninth Edition), 2013
Miscellaneous Clinical Findings
Staphylococcal pneumonia may be associated with rapid illness progression in the presence of treatment, and can result in lung cavitation, pneumatocele, pneumothorax, pleural effusions and empyema.
Tuberculosis is often a diagnosis of exclusion in the absence of available laboratory support. If children have fever for >14 days and clinical pneumonia, health providers should consider tuberculosis. If other causes of fever cannot be identified, then anti-tuberculosis therapy should also be considered based on national epidemiology and guidelines.
Pneumocystis (carinii) jiroveci infection should be considered in HIV-infected children, especially in the setting of hypoxia, respiratory distress and interstitial infiltrates on CXR. Therapy should be tailored accordingly.






